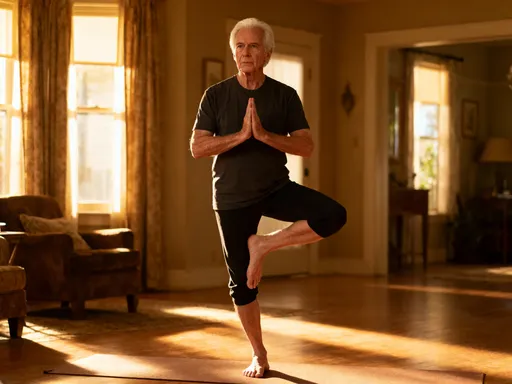
How I Bounced Back Stronger: My Real Talk on Exercise for Recovery
Recovering from an injury or long break can feel overwhelming, but movement is medicine. I learned this the hard way—after weeks of inactivity, simple tasks became struggles. Science shows that the right kind of exercise speeds healing, rebuilds strength, and restores confidence. This is not about pushing hard; it’s about moving smart. Here’s how strategic, gentle training helped me regain what I lost—and how it can help you too.
The Hidden Struggle: Why Recovery Feels So Hard
When the body slows down due to injury, surgery, or prolonged illness, the effects go far beyond physical discomfort. Many people assume that rest is the only path to healing, believing that staying still protects them from further harm. While initial rest is often necessary, extended inactivity can lead to muscle atrophy, joint stiffness, and reduced circulation—making recovery longer and more difficult. The truth is, the body thrives on movement, and without it, even basic functions like climbing stairs or lifting a child can become daunting challenges.
Beyond the physical changes, emotional strain often follows. Feelings of frustration, helplessness, and even isolation are common during recovery. A woman who once managed her household with ease may now struggle to carry laundry up a flight of stairs. A mother who used to play actively with her children might feel too weak or sore to join them. These shifts can erode self-confidence and lead to anxiety about long-term ability. The fear of re-injury becomes a mental barrier, creating hesitation around even the gentlest movements.
Common misconceptions feed this cycle. Many believe that pain means damage, so they avoid any activity that causes discomfort. But not all discomfort is harmful. Distinguishing between the dull ache of rebuilding strength and the sharp signal of injury is crucial. The belief that “more rest is always better” can unintentionally delay healing. Rehabilitation experts emphasize that controlled, intentional movement is not only safe but essential for recovery. The key lies in starting small, progressing gradually, and listening to the body’s signals.
Real-life scenarios vary widely—someone recovering from knee surgery may face mobility limitations, while another adjusting to life after months of bed rest due to illness must rebuild endurance. Office workers who have been sedentary for extended periods may experience chronic back pain or fatigue. Each situation requires patience and a tailored approach. What remains constant is the importance of reintroducing movement in a way that supports, rather than hinders, the healing process.
Science Behind Motion: How Exercise Supports Healing
Movement plays a vital role in the body’s natural repair processes. When tissues are injured, blood flow to the area often decreases, slowing down the delivery of oxygen and nutrients needed for healing. Gentle exercise increases circulation, bringing fresh blood to damaged areas and helping remove waste products that contribute to inflammation. This enhanced flow supports tissue regeneration and reduces swelling, creating an optimal environment for recovery.
Muscle activation is another critical factor. Even mild contractions help maintain muscle mass and prevent the weakening that occurs with disuse. Joints, too, benefit from motion. Synovial fluid, which lubricates joints, circulates more effectively when movement is introduced. This reduces stiffness and improves range of motion, making everyday activities easier over time. Without movement, joints can become tight and less functional, leading to long-term mobility issues.
Controlled physical activity also influences the body’s chemical balance. Exercise stimulates the release of endorphins—natural chemicals that improve mood and reduce the perception of pain. These feel-good hormones can ease the emotional burden of recovery, helping individuals feel more optimistic and resilient. Additionally, regular movement has been shown to lower levels of inflammatory markers in the body, which means less chronic discomfort and a faster return to normal function.
Rehabilitation research consistently supports the idea that the right kind of exercise accelerates healing. Medical professionals agree that early mobilization, when appropriate, leads to better outcomes. However, timing and type matter significantly. Starting too aggressively can cause setbacks, while waiting too long can prolong recovery. The goal is not intensity but consistency—short, manageable sessions that gradually increase in duration and complexity. This balanced approach allows the body to adapt safely and effectively.
It’s important to recognize that healing is not linear. Some days will feel better than others, and progress may seem slow. But each small effort contributes to the larger picture. The science is clear: movement is not the enemy of recovery—it is one of its most powerful allies. By understanding how the body responds to activity, individuals can make informed choices that support their healing journey.
My Turning Point: What Changed My Mind About Moving Again
For weeks after my recovery began, I stayed still—afraid that any movement might undo my progress. I followed doctor’s orders to rest, but over time, I noticed changes I hadn’t expected. My legs felt weak when I stood up. Carrying groceries left me winded. One morning, I tried to lift my youngest child and had to stop halfway, my arms trembling. That moment hit me hard. I realized I wasn’t getting better—I was losing ground.
The turning point came during a routine check-up. My physical therapist asked, “Have you started moving at all?” When I admitted I hadn’t, she explained that while rest was important in the beginning, my body now needed gentle activity to rebuild. She didn’t push me into intense workouts—instead, she suggested short walks and simple stretches. “Your body heals through use,” she said. “Not all discomfort means danger.” That conversation shifted my mindset completely.
I began with just five minutes of walking around the block. The first few steps were stiff, and I felt self-conscious, but I kept going. Within days, I noticed subtle improvements—less stiffness in the mornings, better sleep at night. Those small wins built momentum. I started adding gentle leg lifts while watching TV and seated stretches after meals. Each movement felt like a step toward reclaiming my strength.
Working with a physical therapist gave me confidence. She provided modifications for every exercise, ensuring I stayed within safe limits. She also taught me how to interpret my body’s signals—when to continue and when to pause. Having professional guidance removed the guesswork and reduced my fear of making mistakes. Most importantly, she reminded me that healing isn’t about perfection; it’s about showing up, even in small ways.
That shift—from avoiding movement to embracing it as part of healing—was transformative. I stopped seeing exercise as a threat and began viewing it as a tool for restoration. The emotional boost was just as significant as the physical changes. I felt more in control, more hopeful. My journey wasn’t about bouncing back to who I was—it was about building a stronger, more resilient version of myself.
The First Moves That Actually Helped Me
When starting recovery exercise, simplicity is key. I began with walking—just ten minutes a day, twice a day. It required no equipment, no special space, and could be done at my own pace. Walking improved my circulation, eased joint stiffness, and gave me a sense of accomplishment. Over time, I increased to 15, then 20 minutes, always listening to how my body responded.
Bodyweight squats were another early addition. I started by using a chair for support, lowering myself slowly and rising with control. These helped rebuild leg strength without putting pressure on my joints. Resistance bands became a game-changer—they offered gentle tension to strengthen muscles without heavy weights. I used them for seated rows, shoulder presses, and leg abductions, always focusing on form over speed.
Each exercise was modified to fit my comfort level. If a movement caused sharp pain, I adjusted my posture or reduced the range of motion. I learned that consistency mattered more than intensity. Even on days when I could only manage a few repetitions, I honored the effort. Frequency played a big role—doing short sessions 2–3 times daily was more effective than one long workout.
The benefits showed up quickly. Within a week, I slept more deeply and woke with less stiffness. My mood improved, and I felt more capable in daily tasks. I could carry a basket of laundry without stopping. I played on the floor with my kids again. These weren’t dramatic transformations, but they were real—and they fueled my motivation to keep going.
The key was starting with what felt manageable and building from there. I didn’t compare myself to others or expect rapid results. Instead, I celebrated small victories—like standing longer in the kitchen or walking to the mailbox without discomfort. These moments reminded me that progress wasn’t measured in miles or reps, but in regained independence.
Building a Routine That Fits Real Life
One of the biggest challenges in recovery is making exercise sustainable. I quickly learned that waiting for the “perfect time” meant it would never happen. Instead, I integrated movement into my daily routine. I walked while waiting for dinner to cook. I did seated stretches during morning coffee. While watching evening TV, I used resistance bands or practiced ankle circles. These small habits added up without disrupting my schedule.
Scheduling helped too. I set reminders on my phone for short movement breaks—every few hours, I’d stand, stretch, or take a lap around the house. Pairing exercise with existing habits made it easier to remember and less overwhelming. I didn’t need a gym or special clothes—just the willingness to move, even for a few minutes.
Of course, setbacks happened. Some days I missed my sessions. Others, I felt sore or discouraged. I learned not to treat these moments as failures. Missing a day didn’t erase progress. Soreness wasn’t always a sign to stop—it could mean my muscles were adapting. The goal wasn’t perfection but persistence. I adjusted my routine based on how I felt, sometimes scaling back, sometimes adding a little more.
Progress wasn’t always visible. There were plateaus where I felt stuck. But I reminded myself that healing takes time. I focused on how I felt, not just how much I could do. Could I stand longer? Walk farther? Carry more? These were the real markers of improvement. By prioritizing consistency over intensity, I built a routine that supported long-term recovery without burning out.
When to Push—and When to Pause
Learning to listen to my body was one of the most important skills in recovery. Not all discomfort is the same. A mild ache during or after exercise—especially in muscles—can be a sign of rebuilding. But sharp pain, swelling, or dizziness are warning signs that something is wrong. I learned to distinguish between the two and respond accordingly.
If I felt a sudden, stabbing pain, I stopped immediately. If swelling appeared after activity, I knew I’d done too much. Dizziness or nausea signaled that I needed rest. In those moments, pausing wasn’t giving up—it was protecting my progress. I gave myself permission to scale back, take a day off, or switch to a gentler activity.
Consulting a healthcare provider when unsure was essential. If pain persisted beyond 24 hours or worsened over time, I reached out to my physical therapist. They helped me adjust my routine and rule out complications. Normalizing these conversations removed shame and kept me safe.
I also learned that recovery isn’t about pushing through pain. It’s about honoring the body’s limits while gently challenging them. Some days called for effort; others demanded rest. Adjusting my plan based on how I felt each day wasn’t inconsistency—it was wisdom. This balance allowed me to progress steadily without setbacks.
Beyond Strength: The Unexpected Wins of Rehab Exercise
The benefits of recovery exercise went far beyond physical strength. As my body grew stronger, so did my mind. I noticed sharper focus, better concentration, and a calmer emotional state. The routine gave me a sense of purpose and control during a time when so much felt uncertain. Each small movement became an act of self-care, a quiet promise that I was worth the effort.
Emotional resilience grew alongside physical recovery. The patience required to heal slowly taught me compassion for myself. I stopped rushing, stopped comparing, and started appreciating progress in all its forms. The journey wasn’t just about regaining function—it was about rebuilding confidence and trust in my body.
Independence returned in meaningful ways. I could prepare meals without fatigue, drive without discomfort, play with my children without hesitation. These everyday freedoms, once taken for granted, now felt like gifts. The mental clarity and emotional stability I gained were just as valuable as the physical changes.
Looking back, I see that recovery wasn’t just about exercise—it was about mindset. Patience, self-compassion, and consistency were as important as reps and sets. Healing isn’t linear, and there were days I wanted to quit. But every step forward, no matter how small, counted. I didn’t return to who I was—I became someone stronger, wiser, and more aware of my body’s needs.
Healing isn’t just about waiting—it’s about moving forward with intention. Exercise, done right, becomes a quiet act of self-respect. It rebuilds more than muscle; it restores trust in your body. While every journey is unique, the core truth remains: gentle, consistent effort creates real change. This isn’t a quick fix—it’s a lasting return to living fully. Always consult a healthcare provider before starting any new routine, especially post-injury. Your body’s comeback starts not with a sprint, but with a single, mindful step.