How I Fixed My Back Pain with This Simple Daily Routine
I used to wake up with a stiff lower back and spend my days shifting in chairs, desperate for relief. I’m not a doctor, but after years of discomfort, I found a game-changer: gentle daily movement. Turns out, protecting your spine doesn’t require intense workouts or expensive gear. It’s about consistency, not complexity. This is the simple, science-backed routine I tested and stuck with—no fancy terms, no pain, just real results. If your back’s been whispering (or shouting) for help, this one’s for you.
The Hidden Crisis of Modern Back Pain
Back pain, particularly in the lower region, has quietly become one of the most common health complaints across the developed world. It is not an issue reserved for the elderly or those with physically demanding jobs; it affects office workers, parents, and homemakers alike. In fact, according to data from the Global Burden of Disease study, lower back pain is the leading cause of disability worldwide, surpassing conditions like heart disease and depression in terms of years lived with disability. For many women between the ages of 30 and 55, the burden is even greater due to lifestyle factors such as prolonged sitting, caregiving responsibilities, and hormonal shifts that can influence joint and muscle health.
The rise in back pain correlates closely with modern living. Most adults now spend more than eight hours a day in a seated position—whether at a desk, in a car, or on the couch. This sedentary behavior places continuous pressure on the lumbar spine, disrupting its natural curvature and weakening the muscles designed to support it. Over time, this leads to stiffness, inflammation, and chronic discomfort. Poor posture compounds the issue. Slouching forward while working on a laptop or craning the neck to look at a smartphone creates what experts call “text neck” and “tech back,” conditions rooted in repetitive strain and misalignment.
Another often-overlooked contributor is the lack of varied movement throughout the day. The human body was not designed for static positions. Our ancestors walked long distances, bent, lifted, and squatted as part of daily survival. Today, many people go hours without standing, let alone stretching or shifting weight. This lack of motion reduces blood flow to spinal tissues and limits the nourishment of intervertebral discs, which rely on movement to absorb nutrients. Without regular loading and unloading, these discs can dehydrate and lose resilience, increasing the risk of bulging or herniation.
What makes back pain especially insidious is its gradual onset. Unlike an acute injury, such as a sprained ankle, spinal strain often develops slowly, making it easy to ignore until it becomes debilitating. Many people adapt by modifying their movements—avoiding bending, reducing activity, or relying on painkillers. While these strategies may offer temporary relief, they do not address the root cause. The real solution lies not in masking symptoms but in reversing the habits that created them. Prevention, not just treatment, must become the priority.
Why Your Spine Needs Movement, Not Rest
For decades, the default advice for back pain was rest—stay off your feet, avoid movement, and let the body heal. But modern research has turned this idea on its head. While short-term rest may be necessary after a severe injury, prolonged inactivity often worsens back problems. When muscles are not used, they weaken. The core, glutes, and back extensors all lose tone, reducing the spine’s natural support system. Without muscular stability, the burden of movement shifts to passive structures like ligaments and discs, which are not designed to bear constant load.
Movement is not just beneficial for the muscles—it is essential for the health of the spine itself. The intervertebral discs, which act as shock absorbers between the vertebrae, do not have a direct blood supply. Instead, they rely on a process called imbibition to receive nutrients and expel waste. This process works like a sponge: when pressure is applied to the disc during movement, fluid is squeezed out; when the pressure is released, fresh fluid is drawn back in. Without regular motion, this cycle slows or stops, leading to disc dehydration and decreased flexibility. Over time, this increases the risk of degeneration and pain.
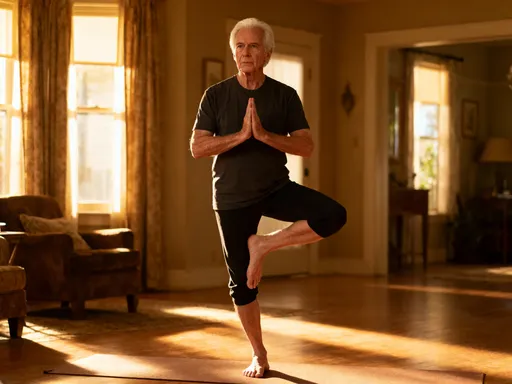
Additionally, movement helps maintain joint mobility and reduces stiffness in the facet joints of the spine. These small joints guide spinal motion and can become inflamed or restricted when not used. Gentle, rhythmic movements such as walking, stretching, or yoga encourage lubrication and prevent adhesions from forming. They also stimulate the production of synovial fluid, which nourishes cartilage and keeps joints moving smoothly.
Perhaps most importantly, movement signals safety to the nervous system. Chronic back pain is not always due to structural damage; sometimes, it is the result of a hypersensitive nervous system that interprets normal sensations as threats. Regular, controlled movement helps retrain the brain to recognize that movement is not dangerous. This concept, known as graded exposure, is a cornerstone of modern pain rehabilitation. By moving consistently and gently, individuals can reduce pain sensitivity and regain confidence in their bodies.
The takeaway is clear: movement is medicine for the spine. It strengthens supporting muscles, nourishes discs, lubricates joints, and calms the nervous system. Rather than fearing movement, people with back pain should learn to embrace it—starting slowly, respecting limits, and building tolerance over time.
The Core Truth: It’s Not Just About Abs
When people think of core strength, they often picture toned abdominal muscles or someone doing hundreds of crunches. But true core stability involves much more than surface-level aesthetics. The core is a complex system of deep muscles that work together to support the spine, pelvis, and torso. Key players include the transverse abdominis—the deepest abdominal layer that acts like a natural corset—the multifidus muscles along the spine, the pelvic floor, and the diaphragm. These muscles form a cylinder of support that stabilizes the spine during every movement, from lifting a grocery bag to bending down to tie a shoe.
Weakness or poor coordination in any part of this system can lead to instability. For example, if the transverse abdominis does not engage properly, the lower back muscles may overwork to compensate, leading to strain. Similarly, if the pelvic floor is weak, it can affect posture and increase pressure on the lumbar spine. This imbalance creates uneven loading, which over time can contribute to disc problems, joint irritation, and chronic pain. The issue is not always muscle strength—it’s neuromuscular control, or the brain’s ability to activate the right muscles at the right time.
Many daily habits interfere with proper core function. Wearing high heels, sitting for long periods, and even chronic stress can alter breathing patterns and posture, leading to disengaged core muscles. Shallow breathing, for instance, reduces diaphragm movement and weakens the connection between breath and core activation. Over time, this leads to reliance on secondary muscles, such as those in the neck and shoulders, to stabilize the body—a recipe for tension and fatigue.
The good news is that core retraining is possible at any age. It begins with awareness. Simple exercises like drawing the navel gently toward the spine while breathing normally can help activate the transverse abdominis. This should not involve holding the breath or sucking in the stomach forcefully—those are counterproductive. Instead, the goal is a subtle, sustained contraction that supports the spine without creating tension. Practicing this during everyday activities, such as standing in line or washing dishes, helps build neuromuscular pathways.
Another effective strategy is diaphragmatic breathing. Lying on your back with one hand on the chest and the other on the belly, focus on breathing deeply into the abdomen so that the lower hand rises while the upper hand stays still. This encourages full diaphragm movement, which naturally engages the deep core. Over time, this improves posture, reduces strain on the lower back, and enhances overall stability. The key is consistency—just a few minutes a day can make a noticeable difference.
My Go-To 10-Minute Morning Routine
After years of trial and error, I settled on a simple 10-minute routine that I do every morning—rain or shine. It requires no equipment, takes up little space, and can be done in comfortable clothes. The goal is not to sweat or push limits, but to gently wake up the spine, activate key muscles, and set a positive tone for the day. I’ve shared this routine with friends and family, and many have reported improved mobility and reduced stiffness within just a few weeks.
The first exercise is the pelvic tilt. Lying on your back with knees bent and feet flat on the floor, gently press your lower back into the mat by tightening your abdominal muscles. Then, release and allow a small arch to return. This movement helps restore natural lumbar curvature and activates the deep core. I do 10 slow repetitions, focusing on smooth control rather than speed. This small motion may seem insignificant, but it reestablishes communication between the brain and the muscles that support the spine.
Next is the cat-cow stretch, performed on hands and knees. In the cow position, I inhale while dropping the belly, lifting the chest, and looking slightly upward. Then, as I exhale, I round the spine toward the ceiling, tucking the chin and drawing the belly in—this is the cat position. I repeat this flow for about one minute, synchronizing breath with movement. This stretch improves spinal flexibility, relieves stiffness, and encourages fluid motion between each vertebra. It also gently engages the core and back muscles, preparing them for the day ahead.
The third exercise is the bird-dog. From the same hands-and-knees position, I extend my right arm forward while simultaneously straightening my left leg behind me, keeping both parallel to the floor. I hold for a few seconds, focusing on balance and a stable core, then return to the starting position and switch sides. I aim for 8 to 10 repetitions per side. This movement challenges coordination and strengthens the glutes, lower back, and deep abdominals. It also improves proprioception—the body’s awareness of its position in space—which is crucial for preventing falls and maintaining good posture.
Finally, I perform glute bridges. Lying on my back with knees bent, I press through my heels to lift my hips off the floor until my body forms a straight line from shoulders to knees. At the top, I squeeze my glutes and hold for a few seconds before lowering slowly. I repeat this 12 to 15 times. Strong glutes are essential for pelvic stability and reducing strain on the lower back. Many people with back pain have underactive glutes, which forces the hamstrings and lower back to overwork during daily movements like standing or climbing stairs.
I always emphasize form over speed. Rushing through these exercises defeats the purpose. Each movement should feel controlled and mindful. If I’m short on time, I still do at least a modified version—sometimes just the pelvic tilt and cat-cow. The key is consistency. Doing a little every day is far more effective than doing a lot once in a while.
Staying Strong Through the Day
Morning movement sets the tone, but spinal health depends on habits throughout the day. For many women in their 30s to 50s, daily life involves long stretches of sitting—whether at a computer, in the car, or at the kitchen table. Without intervention, these hours of inactivity undo the benefits of morning exercise. The solution is not to eliminate sitting but to interrupt it with regular movement and posture resets.
One of the most effective strategies is the “every hour rule.” I set a gentle reminder on my phone to go off every 60 minutes. When it chimes, I stand up, stretch, and do a quick posture check. I roll my shoulders back, lift my chest, and gently tuck my chin to align my head over my spine. Then, I march in place for 30 seconds or do a few seated knee lifts if I’m in a public space. This simple habit improves circulation, reduces muscle fatigue, and prevents the slow creep of poor posture.
At my desk, I’ve made a few ergonomic adjustments. I use a chair with lumbar support or place a small cushion behind my lower back to maintain the spine’s natural curve. My computer screen is at eye level so I don’t have to look down, and my feet rest flat on the floor or on a footrest. If I’m on a call, I often stand or pace—a habit that adds incidental movement to my day. Even small changes, like getting up to refill my water glass or walking to a colleague’s desk instead of sending an email, make a difference over time.
I’ve also learned to be mindful during household tasks. Bending to pick up laundry or lift a child can strain the back if done incorrectly. Instead of rounding my spine, I squat with bent knees and keep my chest lifted, using my legs to power the movement. When carrying groceries or laundry baskets, I engage my core and avoid twisting at the waist. These adjustments may feel deliberate at first, but they become second nature with practice.
Another helpful tip is to incorporate movement into routine activities. While brushing my teeth, I stand on one leg to improve balance. While waiting for the kettle to boil, I do a few gentle side bends or shoulder rolls. These micro-movements add up, keeping joints lubricated and muscles active without requiring extra time. The goal is not to add more to an already full schedule, but to weave movement into what I’m already doing.
When to Pause and Seek Help
While movement is a powerful tool for managing and preventing back pain, it is not a cure-all. There are times when discomfort signals a need for professional evaluation. Certain symptoms should never be ignored. If pain radiates down the leg, especially below the knee, or is accompanied by numbness, tingling, or weakness in the foot, it could indicate nerve involvement, such as sciatica or a herniated disc. Similarly, loss of bladder or bowel control is a medical emergency and requires immediate attention.
Pain that worsens at night or does not improve after several weeks of consistent self-care should also prompt a visit to a healthcare provider. While most cases of back pain are mechanical and resolve with time and movement, some conditions—such as spinal stenosis, spondylolisthesis, or inflammatory arthritis—require specific diagnosis and treatment. Imaging studies like X-rays or MRIs may be needed to rule out structural issues.
It’s also important to recognize when emotional factors play a role. Stress, anxiety, and poor sleep can amplify pain perception. Chronic pain often involves a complex interplay between physical and psychological factors. A healthcare provider can help determine whether a multidisciplinary approach—including physical therapy, counseling, or pain management—is appropriate.
Seeking help is not a sign of failure. On the contrary, it is an act of self-respect. A physical therapist, for example, can assess movement patterns, identify muscle imbalances, and design a personalized exercise program. They can also teach proper techniques for lifting, bending, and sitting—skills that are often overlooked but vital for long-term spinal health. The goal is not to eliminate movement but to do it safely and effectively.
Building a Lifetime Habit, Not a Quick Fix
The most profound change I’ve experienced is not just the reduction in pain, but a shift in mindset. I no longer view movement as a chore or a punishment for past inactivity. Instead, I see it as an act of care—a daily promise to myself to stay strong, mobile, and independent. This shift didn’t happen overnight. It grew from small, consistent actions that gradually became part of my identity. I didn’t need a dramatic transformation; I needed sustainable habits.
Back health, like all aspects of wellness, is cumulative. The 10 minutes I spend each morning may seem insignificant, but over a year, that’s more than 60 hours of dedicated care. These minutes build resilience, improve posture, and reduce the risk of future injury. They also create a positive feedback loop: the better I feel, the more motivated I am to continue. Over time, the routine has become less about fixing pain and more about maintaining vitality.
This approach is especially valuable for women in midlife, who may face additional challenges such as hormonal changes, weight shifts, and increased caregiving demands. Prioritizing spinal health is not selfish—it enables greater energy, mobility, and presence in daily life. Whether playing with grandchildren, traveling, or simply enjoying a walk in the park, a healthy back supports a full and active life.
The journey is not about perfection. There are days when I skip the routine or sit too long at the computer. But I’ve learned to respond with kindness, not criticism. I simply return to the practice the next day. Progress is not linear, but persistence pays off. By treating movement as self-care rather than a task, I’ve built a habit that lasts.
In the end, the spine is not just a stack of bones—it is a dynamic, living structure that thrives on attention and motion. The routine I’ve shared is not a secret cure, but a practical, science-informed way to honor that truth. It requires no special skills, no expense, and no major time commitment. It asks only for consistency, awareness, and a willingness to listen to your body. If your back has been sending signals, consider this your invitation to respond—with movement, with care, and with hope.